ULCER to CKD
•Low backache since 1 week
•Loss of appetite since 1 week
•Facial puffiness since 1 week
•Shortness of breath (class-III) since 1 week
HISTORY OF PRESENTING ILLNESS
Before 20yrs- ACCIDENT- BULLOCK CART RAN OVER HIS ABDOMEN -SURGERY- SPLENECTOMY , 4 PRBC TRANSFUSION
•In 2019–
•The patient was apparently a symptomatic two years back when he had an injury to the DORSUM of the RIGHT FOOT leading to ulceration.
•He went to the local hospital for the same and on doing some investigations he was found to be anaemic (5- HB). He was then referred to Khammam as they could not treat him locally.
•In Khammam, on further investigations – RFT, USG he was told to have a kidney infection due to SEPSIS from the ULCER.(?AKI due to SEPSIS)
•There he had 4 PRBC transfusion and complete debridement of the ulcer along with graft placement.(SPLIT SKIN GRAFTING)
October, 2021 –
•he was apparently alright when he developed-FEVER, COLD, PEDAL EDEMA (PITTING TYPE) , GENERALISED WEAKNESS OF THE BODY.
•He was then taken to a hospital in Suryapet where he was diagnosed with chronic kidney disease and hypertension.
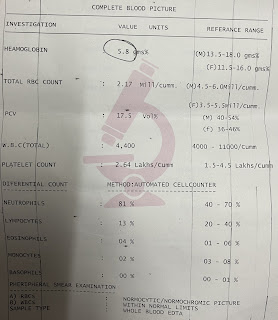
•INVESTIGATIONS DONE- SERUM CREAT, CBP, USG ABDOMEN & PELVIS, CUE
•Treatment given here – injection erythropoietin , tab.nodosis , tab.vitamin D3, tab.neurobion forte, tab.paracetamol
The symptoms subsided in 3 to 4 days. They continued the medication for one and half month and didn’t know whether to refill the medication or not.
•DECEMBER,2021–
•On 15/12/21 – after couple of days of stoppage of the medication that is a week back he developed – low backache, loss of appetite, SOB grade 3, facial puffiness, pedal edema (pitting type) which is when they presented to the OPD.
Addictions- chronic alcoholic since -40 yrs-90ml/day, chronic smoker since -40 yrs, 1 pack 20beedis/day, stopped 2 months back
•Diet- mixed
•Bowel and bladder movements- regular , normal I/o
•Sleep-adequate
•Appetite- reduced since 1 week
GENERAL EXAMINATION
Pt is c/c/c.
•Vitals- BP-150/100MM HG; PR-83BPM; RR-20CPM; TEMP-AFEBRILE
•PALOR-PRESENT ; ICTERUS-ABSENT ; CLUBBING-ABSENT; LYMPHADENOPATHY-ABSENT; EDEMA-PRESENT 1 WEEK BACK, ABSENT NOW.
•Pt is skinny and poorly nourished and has dry skin.
CVS- S1S2 HEARD, NO MURMURS, JVP-
•RS-BAE+, NVBS +
•CNS- NO FND, HMF INTACT
•P/A- SOFT, NON-TENDER, BS +
CKD WITH K/c/o HTN



















Comments
Post a Comment